
Laser Therapy for Concussion
By Benjamin Yuen DC MSc MCC(UK); Fred Kahn MD FRCS(C); and Fernanda Saraga PhD
Features Clinical Techniques“Thank you for giving my son back to me.”
“Thank you for giving my son back to me.”
Four years after an unsuccessful bicycle trick knocked this young man unconscious, he was still suffering from frequent headaches, stiff neck, disturbed sleep patterns, poor concentration and irritability. He dropped out of school, lost his part-time job, started drinking and generally sinking into a form of depression. He had all the signs and symptoms of a mild traumatic brain injury, also known as post-concussion syndrome, and was sliding down a slippery slope of self-destruction. Over a period of six months, the patient received a course of Low Level Laser Therapy treatments, which resulted in a complete turnaround in the patient’s outlook of life. He re-enrolled in school and was doing very well with his school work. He had resumed a part-time job and also his trick cycling. His mother expressed her appreciation for this complete change: “Thank you for giving my son back to me.” Today, he appears to be a happy and healthy 20-year-old.
MILD TRAUMATIC BRAIN INJURY AND POST-CONCUSSION SYNDROME
Within the next hour, six Canadians will suffer a traumatic brain injury.1 Traumatic brain injury (TBI), also known as an intracranial injury, is thought to occur when an external force injures the brain, either through direct impact or by acceleration/deceleration alone. Concussions, or other forms of mild TBIs, make up 75 per cent of all brain injuries.2 In addition to the initial damage caused at the moment of impact, brain trauma can cause secondary injuries, in which a series of events takes place, in the minutes and days following the trauma. These processes, which include alterations in cerebral blood flow, poor oxygenation and heightened intracranial pressure, contribute substantially to the damage from the initial injury.
Symptoms of TBI are diverse and complex and vary with the degree of injury, namely mild, moderate or severe. They can also have a delayed onset of minutes or even days, following the injury. Usual complaints for mild TBIs include headaches, neck pain with stiffness, dizziness, nausea, poor balance, fatigue, apathy, light and sound sensitivity, visual disturbances, amnesia, emotional lability (crying, talkative), cognitive impairment (slow reaction time, memory loss) and difficulty with mental focus and concentration.3,4 Traumatic brain injuries are a growing concern with more than 1.3 million Canadians living with brain injuries today.5
Concussion Facts:
- One does not have to lose consciousness in order to be diagnosed as suffering from concussion.
- A concussion rarely has ‘visible’ brain structural injury; CT or MRI scans are often normal and symptoms are not proportional to the severity of the TBI.
- There are many tests used to assess the severity of a brain injury including the Glasgow Coma Scale (GCS), the Sport Concussion Assessment Tool (SCAT) or the Acute Concussion Evaluation (ACE). Some surveys are being used on the field to determine if athletes should return to play following an injury.
- Previous concussion sufferers are more susceptible to severe symptoms following an additional episode.
- Repeated concussions increase a person’s risk, in later life, for dementia, Parkinson’s disease and depression.6
Today, no single definition of concussion or TBI is universally accepted.7 Intracranial haemorrhages of various types make it even more confusing.8,9 There exist no less than 40 different systems to measure the severity or grade of head injury with little agreement between them.10 Up to 80 per cent of patients that have suffered a traumatic brain injury may develop post-concussion syndrome11 no matter how mild the original injury may have been.
Recent research presented at the 4th International Consensus Conference on Concussion in Sports in 2012 suggested that repeated mild traumatic brain injuries can result in cerebral atrophy and long-term damage to the brain stem and corpus callosum known as chronic traumatic encephalopathy.12
CONVENTIONAL TREATMENTS
Depending on the severity of the injury, the treatment required may be minimal or may include interventions such as medications and emergency surgery (decompression). Within the first few hours following injury, the primary aim of medical personnel is to stabilize the patient and focus on preventing further damage. While there is a tremendous focus on education for the prevention of concussion, there is minimal effort expended to reverse the damage caused by the initial trauma. Physical, speech and occupational therapy may be employed in the rehabilitation process, although complete recovery is not universally achieved in moderate or severe cases. Chiropractors have played a key role in the treatment of the musculoskeletal conditions that are often associated with these injuries, including whiplash, subluxation, neck strain, facet syndromes and muscle spasms. Current research shows that TBI symptoms and whiplash associated disorder (WAD) symptoms are very similar and may delay proper diagnosis and treatment.
LASER MEDICINE FOR NEUROLOGICAL CONDITIONS
For more than 40 years, Low Level Laser Therapy (LLLT) has been effectively used in the treatment of acute and chronic conditions, including degenerative disc disease, repetitive stress injuries, muscle strains, sprains and arthritis.13 LLLT is a non-invasive, pain-free, light-based therapy that uses a combination of red and infrared light in the form of superluminous light-emitting diodes and laser diodes. The power output of these devices is below the level of surgical or other high-intensity lasers. Photon particles of light are absorbed by the mitochondria through cytochrome c oxidase and result in increased cellular ATP levels.13 The neurometabolic cascade of concussion ultimately results in an inadequate supply of ATP to the damaged tissue. The ionic imbalance that results from this depleted ATP, can produce neuronal damage and cellular dysfunction.14 LLLT, therefore has a unique opportunity to supply the brain with increased ATP production during a time when this help is most needed.
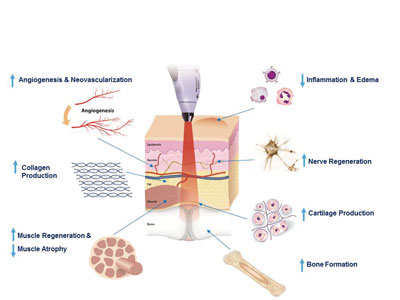
In the case of neuropathic pain, LLLT has been proposed to mediate analgesia by releasing local neurotransmitters such as serotonin15, promoting the release of endorphins16 and through its potent anti-inflammatory effect.17 LLLT has been well documented to stimulate tissue regeneration including angiogenesis, collagen production, muscle and nerve regeneration, cartilage production and even bone formation (See Figure 1).13
 |
|
| Figure 1: Clinical effects of laser therapy.
|
In recent years, research in the field of LLLT has provided some promising pre-clinical evidence to support the use of this technology for the treatment of post-concussion syndrome. In an animal model of acute TBI, mice treated with LLLT showed significant improvement in motor behaviour and reduction in mean lesion size.18 In another animal model of moderate-to-severe TBI, mice treated with LLLT demonstrated significant improvement in the Neurological Severity Score in as little as five days post-treatment and continued to improve over the course of the follow-up, compared to sham-treated controls.19
In humans, a number of individual cases have been documented in which patients with chronic mild TBI showed marked improvement in cognition, executive function, memory and sleep with light emitting diode (LED) treatments.20 These patients may require continuing treatment to maintain and enhance these improvements. It is hypothesized that an overall protective response occurs with repeated LED treatment and that the therapy may reduce the oxidative damage and chronic inflammation that occurs in the brain following TBI, in addition to increasing cerebral blood flow.18,19
The effects of trauma to the cervical spine are often overlooked. The brain stem extends through the atlanto-occipital junction and provides nerve connections between the motor and sensory systems from the central part of the brain to the entire body. It also regulates the central nervous system, and is pivotal in maintaining consciousness and regulating the sleep cycle, heart rate, breathing and metabolism. Mild TBI and cervical dysfunction often go hand in hand. LLLT has been effectively used to treat acute and chronic neck pain.20,21,22 Treatment of the cervical spine may positively affect the brain stem, cerebrospinal fluid and blood circulation of the cerebral hemispheres, thereby reducing the effects of the initial trauma.
CHRONIC POST-CONCUSSION SYNDROME CASE
A 64-year-old woman presented with post-concussion syndrome 10 years subsequent to a motor vehicle accident. She experienced a number of post-concussion symptoms following the accident including cognitive impairment, visual disturbances, headaches, dizziness, fatigue, irritability, numbness/tingling, emotional instability and sensory deficits. She was also experiencing severe pain in her cervical and lumbar spine including right-sided sciatic pain which she described as “knife-like”. A course of LLLT over a period of eight weeks – during which no concomitant therapy was being performed – eliminated or, in the case of some symptoms, markedly improved the severity of her symptoms as documented by the Pain Visual Analogue Scale23 (severity of pain rated on a scale of one to 10) and the Post-Concussion Symptom Scale (in which the patient reports the severity of 22 symptoms on a scale of 0 (none) to six (severe)). The application of the treatment was focused on the cervical and lumbar spine regions and used a combination of superluminous diode arrays (red light, 750 mW and infrared light, 1500 mW) and a laser probe (infrared light, 180 mW).
The patient’s pain levels steadily decreased over the course of treatment. An initial pain level of none was reduced to a three by the end of the course of treatment. Her overall score on the Post Concussion Symptom Scale (mentioned above) was initially 73/132. This was reduced by 83 per cent to a score of 12/132 by the end of treatment. Several symptoms that she had initially rated in the severe category were reduced to mild or non-existent levels, including dizziness, fatigue, feeling emotional, numbness or tingling, feeling mentally foggy and difficulty concentrating.
CONCLUSION
For many years, LLLT has been effectively used to treat patients for a range of musculoskeletal conditions, most notably cervical and lumbar spine conditions, arthritis and repetitive stress injuries. Preliminary scientific research, including animal studies and case reports, along with the case studies presented here, suggests that LLLT may be an effective treatment option for patients with post-concussion syndrome. However, larger controlled studies are warranted to establish this therapy as a viable option for some of the symptoms that patients experience following episodes of trauma to the brain. This technology may provide a therapeutic treatment option to a condition that is in dire need of a solution.
Affiliations: Dr. Yuen is an independent chiropractor and not affiliated with Meditech International Inc. Dr. Kahn and Dr. Saraga are affiliated with Meditech International, the makers of the BioFlex Laser Therapy System.
REFERENCES
1. Ontario Brain Injury Association, www.obia.ca
2. Centers for Disease Control and Prevention (CDC), National Center for Injury Prevention and Control. Report to Congress on mild traumatic brain injury in the United States: steps to prevent a serious public health problem. Atlanta (GA): Centers for Disease Control and Prevention; (2003).
3. Kushner D (1998). “Mild Traumatic Brain Injury: Toward Understanding Manifestations and Treatment” Archives of Internal Medicine, 158(15); 1617-1624.
4. Rees PM (2003). “Contemporary Issues in Mild Traumatic Brain Injury” Archives of Physical Medicine and Rehabilitation, 84(12): 1885-1894.
5. Ontario Brain Injury Association, www.obia.ca
6. Maiese K (2008). “Concussion” The Merck Manual Home Health Handbook.
7. Comper P, Bisschop SM, Carnide N, Tricco A (2005). “A Systematic Review of Treatments for Mild Traumatic Brain Injury” Brain Injury, 19(11): 863-880.
8. Van der Naalt J (2001). “Prediction of outcome in Mild to Moderate Head Injury: a Review” Journal of Clinical and Experimental Neuropsychology, 23(6): 837-851.
9. Savitsky EA & Votey SR (2000). “Current Controversies in the Management of Minor Pediatric Head Injuries” American Journal of Emergency Medicine, 18(1): 96-101.
10. Cantu RC (2001) “Posttraumatic Retrograde and Anterograde Amnesia: Pathophysiology and Implications in Grading and Safe Return to Play” Journal of Athletic Training, 36(3): 244-248.
11. Hall RC, Hall RC and Chapman MJ. (2005) “Definition, Diagnosis, and Forensic Implications of Postconcussional Syndrome” Psychosomatics, 46 (3): 195–202.
12. Kohler R (2012) “Consensus Statement on Concussion in Sport”, http://websitedemo1.com/sca/wp-content/uploads/2012/11/Concussion-in-Sport-Summary-Zurich-2012.pdf
13. Chung H, Dai T, Sharma SK et al. (2012). “The Nuts and Bolts of Low-level Laser (Light) Therapy” Annals of Biomedical Engineering 2012; 40(2):516–533.
14. Marshall CM (2012). “Sports-related Concussion: A Narrative Review of the Literature” J Can Chiropr Assoc 56(4): 299-310.
15. Walker JB. (1983) “Relief from Chronic Pain by Low Power Laser Irradiation” Neurosci Lett 1983; 43:339–344.
16. Yamamoto H, Ozaki A, Iguchi N et al. (1988) “Antinociceptive Effects of Laser Irradiation of Hoku Point in Rats” Pain Clin, 8:43–48.
17. Lim W, Lee S, Kim I et al. (2007) “The Anti-inflammatory Mechanism of 635 nm Light-Emitting-Diode Irradiation Compared with Existing COX Inhibitors.” Lasers in Surgery and Medicine, 39(7):614-21.
18. Oron A, Oron U, Streeter J. et al. (2007) “Low-Level Laser Therapy Applied Transcranially to Mice following Traumatic Brain Injury Significantly Reduces Long-Term Neurological Deficits” J. Neurotrauma, 24:651–656.
19. Wu Q, Xuan W, Ando T et al. (2012) “Low-Level Laser Therapy for Closed-Head Traumatic Brain Injury in Mice: Effect of Different Wavelengths” Lasers in Surgery and Medicine, 44:218–226.
20. Hashmi JT, Huang YY, Osmani BZ, Sharma SK, Naeser MA, Hamblin MR. (2010) “Role of low-level laser therapy in neurorehabilitation” American Academy of Physical Medicine and Rehabilitation, 2(12 Suppl 2):292-305.
21. Chow RT, Johnson MI, Lopes-Martins RA, Bjordal JM. (2009) “Efficacy of Low-Level Laser Therapy in the Management of Neck Pain: a Systematic Review and Meta-Analysis of Randomised Placebo or Active-Treatment Controlled Trials” Lancet, 374(9705):1897-908.
22. Chow RT, Heller GZ, Barnsley L. (2006) “The Effect of 300 mW, 830 nm Laser on Chronic Neck Pain: a Double-Blind, Randomized, Placebo-Controlled Study” Pain, 124(1-2):201-210
23. Lovell MR & Collins MW (1998) “Neuropsychological assessment of the college football player” Journal of Head Trauma Rehabilitation, 13, 9-26.
 |
|
Dr. Benjamin Yuen received his BSc from the University of Toronto and an MSc from Bridgeport University. He completed his chiropractic training at Anglo European College of Chiropractic in Bournemouth, U.K., and has been a practising chiropractor for 34 years. He has also served four years as Director, Post Graduate and Continuing Education Division, at CMCC. Please feel free to contact Dr. Yuen at drbenjaminyuen@hotmail.com or www.alphalaserchiroclinic.com .
 |
|
Dr. Fred Kahn graduated from the University of Toronto and obtained his surgical fellowship in Canada and the United States. For 18 years prior to initiating research in LLLT, he conducted a surgical practice in Southern Calif. and also served as Chief of Staff in Costa Mesa, CA. Dr. Kahn operates Canada’s largest laser therapy clinic with two locations in Toronto. Please feel free to contact Dr. Kahn at fkmd@bioflexlaser.com or www.bioflexlaser.com .
 |
|
Dr. Fernanda Saraga holds an Hon. BSc in physics and a PhD in physiology from the University of Toronto. She has lectured at York University and the University of Toronto. Earlier this year, Dr. Saraga received a travel award at this year’s North American Association of Light Therapy conference for her abstract entitled Low Intensity Laser Therapy for Post-Concussion Syndrome: A Case Study. Please feel free to contact Dr. Saraga at fernanda@bioflexlaser.com.
Print this page