
For the first 15 years of my neurosurgical practice, most of my
patients with spine complaints routinely left the office either
scheduled for surgery or with a prescription for conservative
treatments. These treatments included physiotherapy, traction,
injections, and a host of other treatments too numerous to list.
For the first 15 years of my neurosurgical practice, most of my patients with spine complaints routinely left the office either scheduled for surgery or with a prescription for conservative treatments. These treatments included physiotherapy, traction, injections, and a host of other treatments too numerous to list. But in addition to active therapies, all patients received prescriptions for both a pain medication and a non-steroidal anti-inflammatory (NSAID) capsule. Conservatively, I wrote more than 5,000 of these prescriptions without any thought other than providing relief for my patient’s pain complaints.
However, two events occurred in 2004 that forever changed the way I treat my patients’ non-surgical pain, and what I prescribe for them to take. The first event was very personal. As a triathlete, having participated in more than 70 triathlons, including seven Ironman triathlons, I was accustomed to enduring pain. But I began to have severe left knee pain and took COX-1 NSAIDs, like ibuprofen, for this pain. Over approximately a two-month period, I felt much better but began to have stomach pains, which I found out later was gastritis and early gastric erosion. I became concerned about experiencing this common side effect myself, but also worried about the tens of thousands of patients I had placed on these medications. (I had recently begun to switch many of my patients to the newest COX-2 NSAIDs, but still heard occasional reports about stomach upset.) I considered switching to a different drug, myself, but the next event that sealed how I was going to change my practice, was about to break. On September 30, 2004, the FDA acknowledged the voluntary withdrawal of Vioxx® (rofecoxib), a COX-2 selective NSAID manufactured by Merck & Co.
|
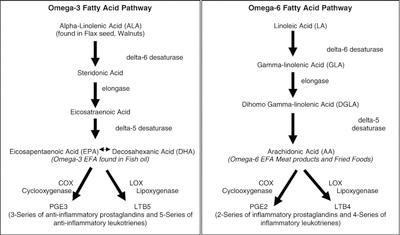
| Graph 1 – Left – Demonstrates the pathway to EPA and DHA concentrated in Fish Oil can produce anti-inflammatory prostaglandins and leukotrienes. Right – Demonstrates the pathway of linoleic acid found in most vegetable oils to arachidonic acid, which produces inflammatory prostaglandins and leukotrienes. Whether inflammatory or anti-inflammatory, it is the balance of these localized cellular hormones that determine the body’s overall level of inflammation.
|
Vioxx and its other COX-2 inhibitor cousins were actually believed to be safer than the COX-1. Because these drugs had gleaned fewer reports of gastrointestinal (GI) side effects, and since there had been no hint of the serious heart and coagulation complications that were now being reported, Vioxx had reached more than nine billion dollars in annual sales in the United States alone! The Vioxx storm started when an increased occurrence of serious cardiovascular events, including myocardial infarction (MI) and strokes, were reported during a clinical trial to determine whether the drug could reduce the risk of colon cancer. It became apparent that besides inhibiting COX-2, these agents selectively interfered with prostacyclin synthesis, a prostaglandin essential in reducing intravascular coagulation, and thus the increased incidence of MI and stroke. Because of persistent significant gastric, and now cardiovascular, side effects, the safety of these pharmaceutical choices was now being called into question.
With the removal of Vioxx from the market, many practitioners now treat NSAIDs with increased caution when prescribing. In 2006, The American Medical Association recommended the following considerations with their use:
- Limit the duration and dosage of the prescribed NSAID and ask about and advise patients on combination NSAID therapy.
- Treat patients with H pylori infection prior to beginning NSAID therapy so as not to increase the risk of complicated ulcers.
- Institute “gastroprotection” for patients at high risk of gastrointestinal complications.
OMEGA-3 FISH OILS – A BETTER CHOICE
Following my own negative experience with NSAIDs and my heightened concern resulting from the Vioxx scare, I was determined to seek out a better choice for providing a reduction in inflammation-induced pain, and also reducing the side effects from medications consumed for months at a time. I began seeking out alternative treatments, and quickly found several hundred peer-reviewed journal articles in mainstream medical journals reporting on the use of omega- 3 essential fatty acids (EFAs) found in fish oil to block the inflammatory response in a similar but safer way as compared to NSAIDs. The majority of these articles had referenced omega-3’s benefits with heart, vascular disease and improving lipid profiles. But several articles referenced the genesis of the omega-3 benefits and how they had a similar function to many NSAIDs of reducing inflammatory prostaglandin production (see Graph 1). EFAs, whether O3 or O6, are required for the production of hormone-like substances called eicosanoids which include thromboxanes, leukotrienes and prostaglandins. Additionally, omega-3s and the types of eicosanoids they produce help to balance the omega-6 eicosanoids associated with the inflammatory response.
The omega-6 EFA, linoleic acid (LA), is a polyunsaturated fatty acid found in many vegetable oils, especially corn oil, poppy seed, safflower and sunflower oils, and is used in the biosynthesis of arachidonic acid (AA), which can form inflammatory prostaglandins. Both omega-3s and omega-6s are incorporated into the bi-lipid membranes of animal cells and act as substrate repository for these localized hormones (eicosanoids). Both are polyunsaturated fatty acids that have two or more double bonds and, in addition to producing the eicosanoids, these EFAs are part of the phospholipids that are necessary for the formation and maintaining integrity of healthy cell membranes, neuronal development, and functioning of the brain and nervous system.
Omega-6s, when consumed in large amounts, such as is common in the Western diet, lead to excessive linolenic acid and increased formation of arachidonic acid, which then forms the pro-inflammatory eicosanoids. Animal proteins, especially red meat, also contain an abundant amount of arachidonic acid.
The anti-inflammatory eicosanoids derived from omega-3s, are found primarily in fish and, to a lesser extent, flax seed, walnuts, and certain algae. A deficiency in omega-3s, especially DHA (docosahexaenoic acid) and EPA (eicosapentaenoic acid), which are the most bioactive, will result in reduced levels of anti-inflammatory eicosanoids. An increase of omega-6 in the diet, versus omega-3, results in an imbalance and, in general, an inflammatory state. The reverse is also true. Increasing your diet with omega-3s or using dietary supplements will help to reduce inflammation. Having researched this supplement, my goal was to use omega-3s as a safer NSAID and treat my own pain as well as my patient’s pain associated with arthritic joints of the spine.
OMEGA-3 EFAs FOR SPINE PAIN
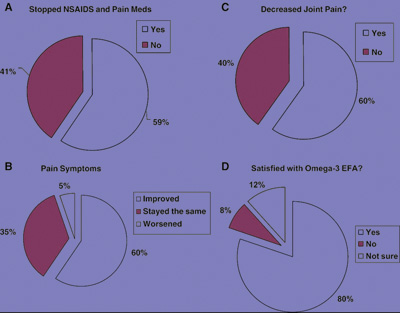
I personally began to take two grams of mixed DHA and EPA fish oil supplements for a two-month period. I had no further knee pain, began to train again, and, importantly, had no further stomach problems. In 2005, I surveyed 125 of my non-surgical spine pain patients to whom I had also recommended taking omega-3 fish oil supplements. The survey showed a surprising result; 60 per cent had obtained significant spine pain relief and almost the same amount – 59 per cent – were able to stop taking pain medications and NSAIDs and just use omega-3 supplements for pain relief! I reported these results in Surgical Neurology, which prompted an editorial from the senior editor to encourage more neurosurgeons to learn about alternative treatments (see Graph 2).
|
| Graph 2 – Results of a survey of 125 respondents on omega-3 EFAs for a minimum of two months who had been seen with non-surgical spine pain.
|
A NEW STRATEGY
For the last five years, I have continued to use omega-3 supplements as the first line of treatment for my patients with non-surgical spine pain, and I continue to receive tremendously positive feedback. As with any supplement, I urge patients to take a high-quality, pharmaceutical grade product, and caution them when taking blood thinners and fish oil, as there is a possibility of an accentuated effect on international normalized ratio (INR) values. In general, however, there are few complaints and most patients are very compliant with these supplements.
Because of continuing problems with pharmaceuticals with respect to withdrawal and black boxes on labels, many patients seek out natural alternatives to drug treatments. It is important to learn about those products that, like omega-3 fish oils, have been researched and have now crossed over to become standard treatments for patients and how they can be integrated with chiropractic to provide optimal pain treatment. You, as the practitioner, can be a better source of information than any commercial advertisement, and you are better equipped to alert them to any potentially harmful interactions. •
Dr. Joseph Maroon, a board certified neurosurgeon at the University of Pittsburgh and team physician to the Pittsburgh Steelers, has become one of the leading advocates of fish oil in the United States. He has recently authored two books, Fish Oil: The Natural Anti-inflammatory and The Longevity Factor: How Resveratrol and Red Wine Activate Genes for a Longer and Healthier Life. Dr. Maroon currently serves as medical advisor for Nordic Naturals. For more information, see www.inflammationsolutions.com.
Print this page