
For every overuse injury, the formula that caused the injury is fairly standard.
For every overuse injury, the formula that caused the injury is fairly standard. The runner did not rest enough between sessions to allow the tissue to heal itself and let the benefit of the training effects on the body to kick in. In essence, the demand the runner has put on the tissue (muscle, tendon, bone) has exceeded that tissue’s capacity to adapt to the training.
 |
|
| Photo: Shutterstock Advertisement
|
A five-kilometre (5K) runner would never train for a marathon by one day deciding to run 42K and trying to maintain that level. They know they would get hurt. Every runner knows that one has to build up to the goal to let the tissues, along with the heart and lungs, adapt to the new training schedule. This is true in every sport – if your demand outweighs your capacity – you will get injured at some point.
The tricky part is determining how much you should increase your training – per run, per week, per month – without exceeding the tissue’s capacity. There are many theories (e.g., 10 per cent per week) but everyone is different in terms of their physiology and genetics – some could increase more than 10 per cent and have no problems, some may increase less than 10 per cent and have several injuries. A runner needs to listen, feel, hear and see what their body is telling them and adjust their training accordingly. Be your own experiment.
Once an injury gets to the point where the runner seeks treatment, it has usually been building for a considerable period of time. As sport chiropractors, we hear, “My (injured area) starts to hurt about 30 minutes into my run. My pain is so bad, I now have to stop running when the pain starts.” In general, the first goal with the runner is to reduce the demand. We don’t recommend that patients stop running completely but they have to cut back so that there is no pain during the run and no pain the next day. If they were getting pain at 30 minutes, we suggest they try 15 or 20 minutes to start. We can also reduce the demand by changing the running surface (asphalt versus trails), running route (always running on the same side of the road/sidewalk versus alternating sides) and running conditions (limit hills, no icy conditions), and by trying pool running.
Once we have established a new baseline for pain-free running, then the second goal is to increase their capacity. Treatment, although based on the diagnosis, is designed to increase the capacity of the tissue to withstand the demand. This, combined with the aforementioned new training program, will increase the tissue’s tolerance. There are other ways to increase the tissue’s capacity, including improving nutrition, decreasing stress, getting better sleep/rest and cross training.
Hydration
The concept of demand and capacity also can be applied to hydration during training. The body has a clear demand when it comes to hydration – a demand that can vary with training intensity, temperature, humidity and sport, to name a few factors. In this case, if the athlete is not meeting the demand, they will become dehydrated, which will affect performance and in some cases lead to heat exhaustion and even death. If, however, the athlete exceeds their capacity (i.e., by drinking too much water during training), they can develop a condition known as hyponatremia, or water intoxication, which also can lead to death.
As a subset of better nutrition and performance, it is imperative that a conversation with respect to hydration occur. Much in the way that the muscles need to be trained to increase their capacity, the digestive system needs to be trained to enhance tolerance. Runners need to train using a hydration strategy that works for them not only technically in terms of how they consume the fluid, but also in terms of what their body can handle comfortably.
For health and performance, it is recommended a person consume fluids before, during and after running to avoid dehydration (water deficit in excess of two to three per cent body mass). While the amount of fluid a runner drinks will vary due to multiple factors as outlined above, the principle remains to replace the fluid lost through sweat during the run. It is not necessary for the fluid intake to match sweat rate, but it is generally recommended the runner get as close to this balance as they comfortably can.
The vast majority of runners can ensure adequate hydration by monitoring the colour of their urine (pale yellow is appropriate). If they are not meeting their demand, their urine will often be a darker and browner colour. If they are overhydrating or exceeding their capacity, their urine will often be almost clear. Runners can avoid either end of the scale by simply listening to their thirst.
 |
|
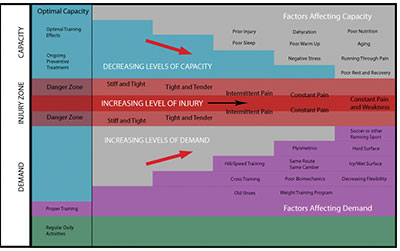
| The Optimal Capacity box shows the best capacity/demand ratio – a high capacity combined with a low demand keeps the runner out of the danger zone. As you increase the number of factors that affect the tissue’s capacity (top area), there is a decreasing level of capacity (top red arrow). Correspondingly, as you increase the number of factors affecting the demand (bottom area) on the tissues, there is an increasing level of overall demand (bottom red arrow). Any combination of these two factors will push the athlete toward the Injury Zone. In the Injury Zone, there is an increasing level of injury from stiff and tight to constant pain and weakness as the capacity decreases and/or the demand increases.
|
Avoiding overuse
Cross training is often recommended to runners and is a viable way to challenge the body in new ways to increase the training effects. The runner has to take into account this extra demand on the tissues though and may have to decrease the running program, at least for a short period of time. When we add new activities and then experience pain, it can be difficult to tell which activity was the last straw – often, it is the combined effect. If the athlete gets pain, they will need to decrease all aspects of their training initially as previously outlined, then progress more slowly, increasing the intensity of each activity one at a time. If there is a consistent increase in pain with the progression of a specific activity, that activity should be evaluated further.
Runners should challenge themselves by adding speed training or hill training into their regimen. Typically, we see runners after this change in training because of the increased range of motion needed to perform them. We need more ankle and hip flexibility for the speed training, and definitely more ankle flexibility for the hills. Even though runners may go back to the same running program they were on prior to the hill or speed training, their capacity will be decreased to the point that injuries can now creep in. They may not always associate the change with their pain, however, because the pain can be delayed for up to two to three weeks after the session.
Talking to the runner about decreasing their demand and increasing their capacity is a simple concept that can drive home your plan for them going forward. As the runner’s pain is alleviated, they will often think during their run that they can keep going beyond the set plan. Although it feels better, if the runner runs far enough or with high enough intensity, the pain will return. Just because a knee, ankle or hip is pain free doesn’t mean it has the capacity to tolerate a large jump in demand.
By sticking to the concept outlined, runners will enjoy a quicker return to their training goals.
Dr. Muir and Dr. Howitt will co-chair the Run Faster conference on Nov. 16 and 17, 2013, in Whitby, Ont.
For more information visit www.rccssc.ca .
 |
|
 |
Dr. Brad Muir is an associate professor at the Canadian Memorial Chiropractic College. He has lectured across Canada on running, hockey and functional testing as well as vibration therapy. You can contact him at bmuir@cmcc.ca.
Dr. Scott Howitt is also an associate professor at CMCC and a sessional lecturer for the University of Guelph. You can contact him at showitt@cmcc.ca or showitt@stjohnsrehab.com.
Print this page