
Worldwide, the proportion of older adults is increasing to the highest number ever recorded.
Worldwide, the proportion of older adults is increasing to the highest number ever recorded. By 2017, there will be more adults aged 65 and older than children under age five, according to the World Health Organization. By 2050, over 20 per cent, or about two billion, of the world’s population will be older than age 60.
As chiropractors, we might expect that the 15 per cent of the chiropractic patient population aged 65 and older presently served will increase, since spine-related musculoskeletal pain is a significant health issue in this age group. It is important to continue to increase public awareness that chiropractic is both safe and effective for many conditions common in older adults, and that manipulation is not a risk factor for vertebrobasilar stroke.
We should also proactively ensure the graduates of our training institutions are well prepared not only to provide relief for musculoskeletal conditions, but also to provide preventive services and promote wellness. This requires that DCs be knowledgeable about the health problems, risk factors and preventive care strategies that will promote successful aging in their patient population.
 |
Successful aging defined
Most definitions of the term “successful aging” involve three components: low probability/presence of disease or disability; high cognitive and physical function; and active engagement in life.
Another way successful aging is conceptualized is through researcher James Fries’s “compression of morbidity” model, in which morbidity is compressed so that one lives a greater period of time free of illness and disability. This model considers “morbidity” to be any impairment of function or decrease in health-related quality of life. Morbidity is essentially related to ability to function, rather than to any specific disease process. This is highly relevant to chiropractic practice, since chiropractic care helps people function better, helping us make a case that chiropractic can contribute to the compression of morbidity.
Successful aging measures
Besides defining “successful aging,” we also need to be able to measure it. In the “compression of morbidity” model, since morbidity is seen as a decrease in normal function or health-related quality of life, measures of functional disability and quality of life can be used as proxies for morbidity.
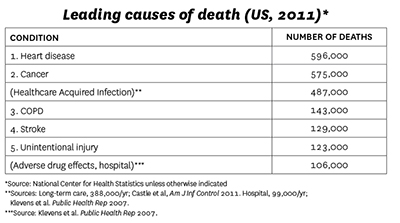
Mortality. Using measures of both mortality and morbidity, we can identify ways in which chiropractic can help people age more successfully. For example, it is instructive to look at overall causes of death. Table 1 shows the leading causes of death in the U.S. for 2011, but additional nonspecific causes have been inserted into the standard list to illustrate an important issue. These numbers show that health-care-acquired infections, primarily from long-term care facilities, are more numerous than any other causes of death, except cancer and heart disease. Furthermore, adverse drug effects in the hospital come in as a leading cause of death after unintentional injury.
Chiropractic care can help people maintain their physical function, as well as help manage pain. This can help them stay independent, avoid nursing homes and, perhaps, hospitalization. In many cases, it could prevent the need for medications for pain.
Morbidity. A substantial number of the leading causes of disability may respond to chiropractic care. The top-ranking conditions contributing to years lived with disability (YLD) are listed below, with those most likely to be improved by chiropractic care shown in bold:
- Low back pain
- Major depressive disorders
- Other musculoskeletal conditions
- Neck pain
- Anxiety disorders
- Chronic obstructive pulmonary disorders
- Drug use disorders
- Diabetes
- Osteoarthritis
- Asthma
Optimizing the effect of chiropractic care
Chiropractic care already plays an important role in decreasing mortality and compressing morbidity. We can increase our effectiveness in compression of morbidity even more by enhancing our ability to help patients to decrease risk factors, practise prevention and change health behaviour.
Chiropractic care is more than manual procedures. It encompasses the entire clinical encounter. DCs routinely provide advice on healthy lifestyle to their patients, and this can be an important factor in helping patients improve their health.
Decrease risk factors. DCs must be aware of patients’ risk factors, and think holistically. Remember that morbidity encompasses multiple conditions (comorbidities) and is a broad term referring to limitation of functional ability. Multiple chronic conditions have become the new normal in older adults. In fact, fewer than 10 per cent of patients aged 65 and older have only one chronic condition, according to data from the U.S. Centers for Medicare and Medicaid Services.
It is essential to assess older adults for the presence of risk factors. All patients should be assessed, at a minimum, for poor diet, lack of physical activity, tobacco use, overweight/obesity (using body mass index or BMI) and blood pressure. Obesity and overweight are readily assessed by calculating the BMI (a BMI of 25-29-9 indicates overweight and a BMI of 30+ indicates obesity).
It is also important to be aware of signs and symptoms of cognitive decline in older adults, as this can have a significant impact on all aspects of their life. The Standardized Mini-Mental State Examination can be used to assess cognitive function. A Canadian resource for this instrument is available from the British Columbia Ministry of Health website.
Another important but often overlooked risk factor for poor health is health literacy. Older adults are especially vulnerable to poor health literacy, which can be compounded by poor eyesight and hearing. It is essential that DCs make sure their older patients understand instructions for home care. Provide them with a handout of instructions with writings large enough to be read easily and written at no more than 8th grade level readability.
Practise prevention. There are three phases of prevention, all of which might occur during a clinical encounter. Primary prevention prevents a disease or injury from occurring at all by removing risk factors. Secondary prevention detects a disease or condition at an early stage in order to intervene by reducing or removing risk factors or providing appropriate treatment. Tertiary prevention reduces or removes the sequelae of an existing condition or injury. It is synonymous with rehabilitation.
A particularly important example of primary prevention for older adults is fall prevention. Approximately one-third of community dwellers over the age of 65 experience a fall. Falls are the leading cause of non-fatal injury in older adults. Of those who are hospitalized due to a fall, 40 to 50 per cent enter a nursing home as a result.
DCs should get a fall history from their older patients and assess their risk for falls. The Timed-Up-and-Go is a simple test that takes only a few minutes to perform and assesses fall risk. The patient stands up from a chair, walks three meters, as quickly and safely as possible, turns around, returns and sits down. If the test takes more than 14 seconds, the patient is at risk for falls. Lower-body strengthening exercises should be recommended to improve balance, along with chiropractic care to manage pain, stiffness and promote optimal function.
Improve health behaviour. Although a healthy diet and avoidance of substance abuse and polypharmacy are essential components of good health, vigorous physical activity is perhaps the “magic bullet” for successful aging. Only 14 per cent of people aged 65 to 74 and seven per cent of those aged 75 to 84 in the U.S. get even the minimum recommended amount of physical activity. DCs should provide all older adults with information on getting recommended amounts of exercise.
As the number of older adults continue to rise, promoting healthy aging is essential not only to the world’s population, but also to its economy.
 |
|
Cheryl Hawk, DC, PhD, CHES is a professor and dean of research at Logan University in Chesterfield, Mo., and author of more than 90 publications in peer-reviewed scientific journals. She was named Researcher of the Year by both the American Chiropractic Association (2003) and the Foundation for Chiropractic Education and Research (2005).
Print this page